
Gene Editing Enzymes
Nucleases for Research and Clinical Applications
There are many commercial nuclease suppliers for basic research and academic purposes. But your goals and needs are different. You aspire to utilize CRISPR gene editing for research or therapeutic purposes and need a product that is going to be available under the appropriate quality systems (research grade, ISO 13485, or full cGMP) as you progress.
Aldevron manufactures and stocks nucleases that can eliminate the need for custom manufacturing runs, as your program moves towards commercialization.
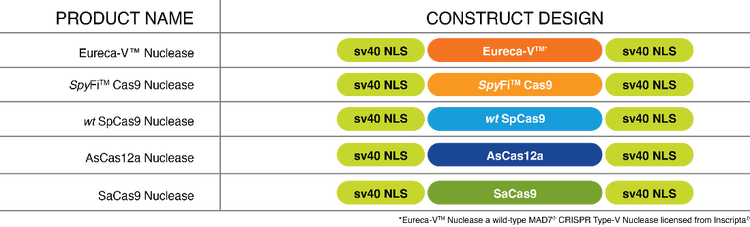
| Product | Description | Stocked at Research Grade | cGMP Pack Sizes | Drug Master File on File |
| Eureca-V™ Nuclease* | Wild-type MAD7™ ® Type-V nuclease with pass-through licensing* | Yes | Coming Soon | No |
| SpyFi™ Cas9 Nuclease | High fidelity nuclease with less off-target activity | Yes | Yes | Yes |
| SpCas9 Nuclease | Wild-type SpCas9 | Yes | Yes | Yes |
| AsCas12a Nuclease | Wild-type AsCas12a | Inquire | No | No |
| SaCas9 Nuclease | Wild-type SaCas9 | Inquire | No | No |
*Licensed from Inscripta®
Ordering Information
| Product | Small Size | Catalog Number | Price | Large Sizes | Catalog Number | Price |
| Eureca-V™ Nuclease | 1MG | 9300-1MG | $2,015 | 5MG | 9300-5MG | $7,575 |
| SpyFi™ Cas9 Nuclease | 0.25MG | 9214-0.25MG | $663 | 5MG | 9214-5MG | $9,523 |
| SpCas9 Nuclease | 0.25MG | 9212-0.25MG | $403 | 5MG | 9212-5MG | $6,957 |
| AsCas12a Nuclease | Inquire | |||||
| SaCas9 Nuclease | Inquire | |||||
| cGMP-Manufactured Nucleases | ||||||
| SpyFi™ Cas9 Nuclease – GMP | 1MG | 9216-0.1ML | 10MG | 9216-1ML | ||
| SpCas9 Nuclease | 1MG | 9211-0.1ML | 10MG | 9211-1ML | ||
Don’t See What You Need?
Aldevron offers custom manufacture of unique Cas enzyme configurations including dCas9 fusions, nickases, Cas9 variants and non-Cas9 nucleases. For more information visit our Custom Protein Manufacturing page or contact our Custom Nuclease Services group.
Ribonucleoprotein Production**
Aldevron offers an RNP service to streamline transforming your CRISPR reagents into therapies. Working with your unique guide RNAs, we’ve defined the optimal conditions for complexing, characterizing, and storing CRISPR RNPs created with Aldevron research and cGMP-grade CRISPR/Cas9 proteins. Our proprietary release panels are compliant with 21CFR210-211 and designed to meet current draft guidance from the FDA regarding gene editing, which provides consistency of the final product.
Learn more about our RNP Production Services
- BROCHURE: Advancing CRISPR-based Therapeutic Development
- WHITEPAPER: Next-Generation CRISPR Approaches: Explore Strategies to Advance Therapeutic Programs Supporting Current Regulatory Guidance
- WHITEPAPER: Expectations on the Pathway to GMP for Gene-Modified Cell Therapies
- CASE STUDY: Enabling Novel CRISPR-Cas9 Delivery: A Case Study Supporting Innovative Genomics Insititute
- WEBINAR: Genome Editing Tools: Beyond Discovery
- WEBINAR: CRISPR Cures 2033: Expanding the Public Health Impact of Gene Editing
- ARTICLE: Expediting IND applications with drug master files
- PODCAST: Insights into the Editing of the Human Genome
Publications featuring other Aldevron Nucleases
- High-efficiency nonviral CRISPR/Cas9-mediated gene editing of human T cells using plasmid donor DNA
This publication showed improved CAR-T knock-in efficiency, reduced cell death, and an improved T cell phenotype for CAR-T cell therapies using Nanoplasmid compared to conventional plasmids and linear DNA as an HDR template. Experiments are conducted with SpyFi Cas9 Nuclease.
Oh SA, Senger K, Madireddi S, Akhmetzyanova I, Ishizuka IE, Tarighat S, et al. High-efficiency nonviral CRISPR/Cas9-mediated gene editing of human T cells using plasmid donor DNA. Journal of Experimental Medicine. 2022;219(5). https://doi.org/10.1084/jem.20211530
- Large-scale GMP-compliant CRISPR-Cas9–mediated deletion of the glucocorticoid receptor in multivirus-specific T cells
This paper showed GMP-compliant method to manufacture CRISPR gene-edited VSTs that are unaffected by glucocorticoid treatment. These CRISPR-edited VSTs have comparable potency to non-gene edited VSTs but could be co-administered to patients with steroids. The GMP manufacturing workflow applies Aldevron SpyFi™ Cas9 Nuclease as the gene editing reagent due to its high on-target editing efficiency and greatly reduced off-target editing in comparison to wild-type SpCas9.
Basar, R., Daher, M., Uprety, N., Gokdemir, E., Alsuliman, A., Ensley, E., Ozcan, G., Mendt, M., Hernandez Sanabria, M., Kerbauy, L. N., Nunez Cortes, A. K., Li, L., Banerjee, P. P., Muniz-Feliciano, L., Acharya, S., Fowlkes, N. W., Lu, J., Li, S., Mielke, S., Kaplan, M., … Rezvani, K. (2020). Large-scale GMP-compliant CRISPR-Cas9-mediated deletion of the glucocorticoid receptor in multivirus-specific T cells. Blood advances, 4(14), 3357–3367. https://doi.org/10.1182/bloodadvances.2020001977


